Reasons to Become a Cardiac Perfusionist
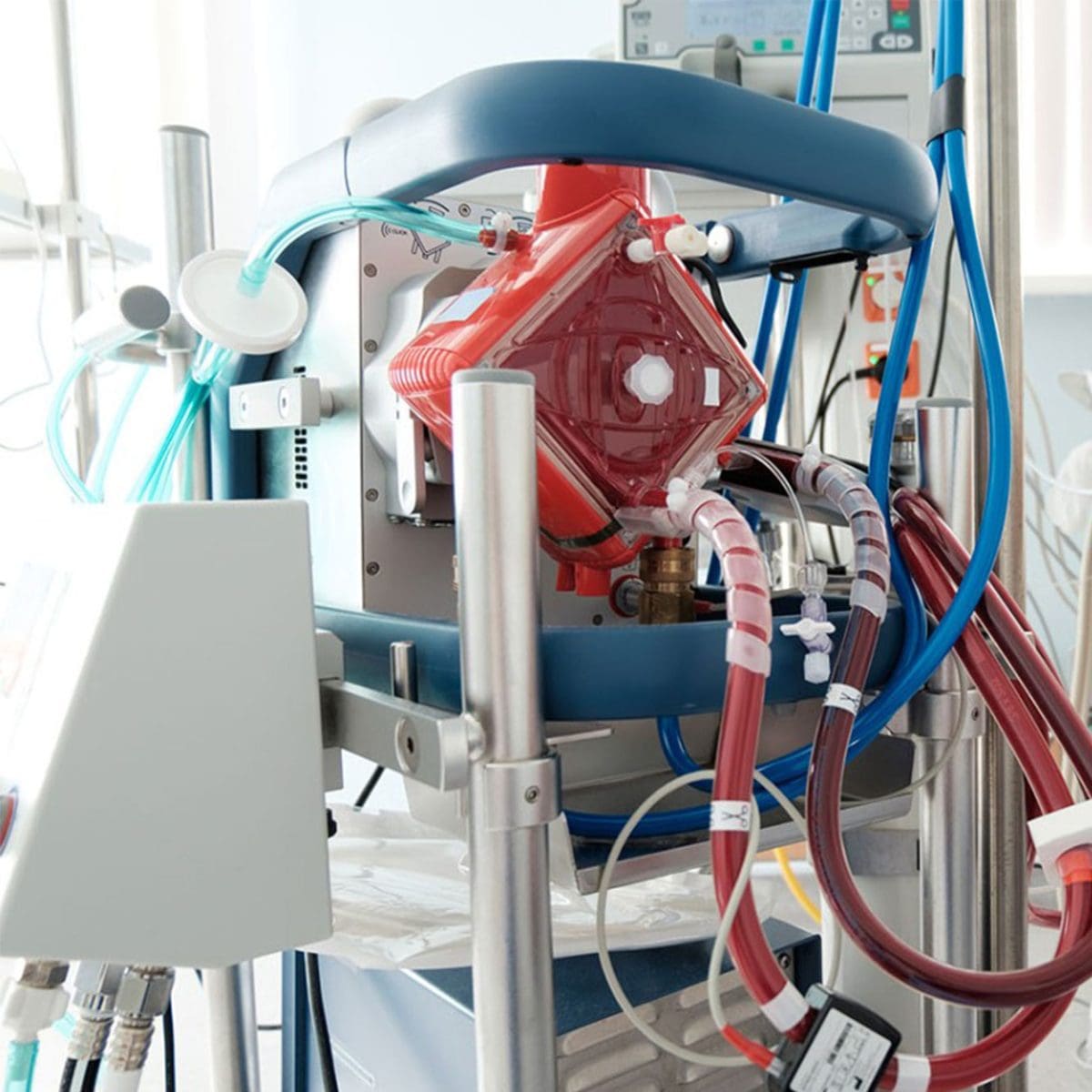
Are you considering becoming a cardiac perfusionist, but are just not sure if it is the right career path for you? No worries, we are Vivacity Perfusion and are here to guide you through the top reasons why joining the world of perfusion will become one of the best career choices you make. Not only will you have the opportunity to save countless lives including children and adults, but you will make an impact on all of those around you.
Not only is there a high demand for cardiac perfusionists, but we at Vivacity are also always looking to add more perfusionists to our team and be a part of your journey to get you working in a hospital. According to the 2021 annual report from abcp.org, only 210 examinations were administered and certified to become a clinical perfusionist (CCP). Out of 245 million adults in the United States, 210 is a minuscule number. So what is stopping you from being a cardiac perfusionist? Not only will you have job security, but you will have a competitive salary in the healthcare industry and be able to change lives each and every day.

Let’s continue on and dive into the details and top reasons you should become a cardiac perfusionist.
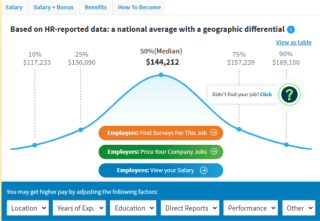
The Competitive Pay Benefits
The average salary of a licensed perfusionist is over $130,000 per year, and if you are a traveling perfusionist you can expect to make over $210,000 per year nearly doubling your salary. On top of that, you will have a relatively low cost of education compared to other healthcare professionals. The average cost of tuition for a perfusionist is about $65,000. As you can see, traveling perfusionists make more per year. At Vivacity Perfusion, we specialize in contracting perfusionists in hospitals around the United States. That means if you are a perfusionist and want to increase your salary, reach out to us at Vivacity Perfusion for traveling perfusion opportunities.
Training Is Short
According to the American Academy of Cardiovascular Perfusion, a truly effective perfusion training program will require a bachelor’s degree. However, if you have a bachelor’s degree in the sciences already, then you can be well on your way to applying to a two-year program.
Do You Feel That Traveling Perfusion is for You?
If you are a licensed perfusionist or on the path to becoming a certified perfusionist wanting to travel and double your salary, contact us at Vivacity Perfusion to see how we can help you today. We hope that this information was helpful for y ou as you continue to further your career in perfusion, or as you just start out. Vivacity Perfusion accepts travelers to apply once they have at least two years of experience post-graduation. If you are interested in learning more about what we do at Vivacity Perfusion or getting contracted please reach out to [email protected] for more information.
ou as you continue to further your career in perfusion, or as you just start out. Vivacity Perfusion accepts travelers to apply once they have at least two years of experience post-graduation. If you are interested in learning more about what we do at Vivacity Perfusion or getting contracted please reach out to [email protected] for more information.